In Brief
Deciding to join an insurance panel can feel like you’re choosing sustainability for your practice. Insurance acceptance opens doors to new referrals, helps steady your caseload, and allows clients who can’t afford out-of-pocket therapy to see you. In theory, it should be straightforward: you’re a licensed professional, there’s a desperate shortage of mental health providers, and insurers need networks that meet demand.
And yet the process feels designed to wear you down. Panel applications often take three to six months to process (and sometimes longer). What’s more, according to a 2019 report published by the U.S. Department of Health and Human Services, roughly 42% of behavioral health providers say they’ve struggled with insurance credentialing. The requirements are rarely published in plain language, leaving you to guess what counts as “complete.” And silence from insurers isn’t an oversight; it’s the default.
The question isn’t just why it takes so long, but how you can move through the slog with fewer stalls and more strategy.
Why Insurance Credentialing Takes So Long
Credentialing is, technically, about verifying your legitimacy: your license, training, insurance, history. Insurers will tell you they’re protecting clients and reducing fraud. But that story misses how much of the bottleneck is simply bureaucratic drift, including:
- Administrative backlog. Insurers process thousands of applications a month. Credentialing departments are small. Every missing box can set you back weeks.
- Verification requirements. Education, licensure, malpractice insurance, and references all must be checked directly by insurers. That means waiting on your grad program, your supervisor, or a reference to answer their phone.
- Panel “closures.” You may hear that a panel is “full.” But “full” is often flexible, especially if you serve children, accept Medicaid, or practice in underserved zip codes.
- State regulation limits. Some states impose rules meant to rein in credentialing delays: California is in the process of passing AB 1041, which requires completed credentialing determinations within 90 days of receiving a completed application. Illinois law requires determination completion within 60 days, and Kentucky has an “Any Willing Provider” law, meaning that insurers must accept qualifying providers who meet participation terms. But compliance is uneven, and many therapists don’t even know the law is on their side.
The consequence isn’t just annoyance, it’s delayed access for those seeking help. According to a 2023 survey by the Kaiser Family Foundation, nearly half (43%) of insured adults who rated their mental health as “fair” or “poor” were unable to receive necessary mental health services. That met with provider shortages mean clients wait months for therapy. Insurance panel bottlenecks only make that worse.

What Insurers Really Require
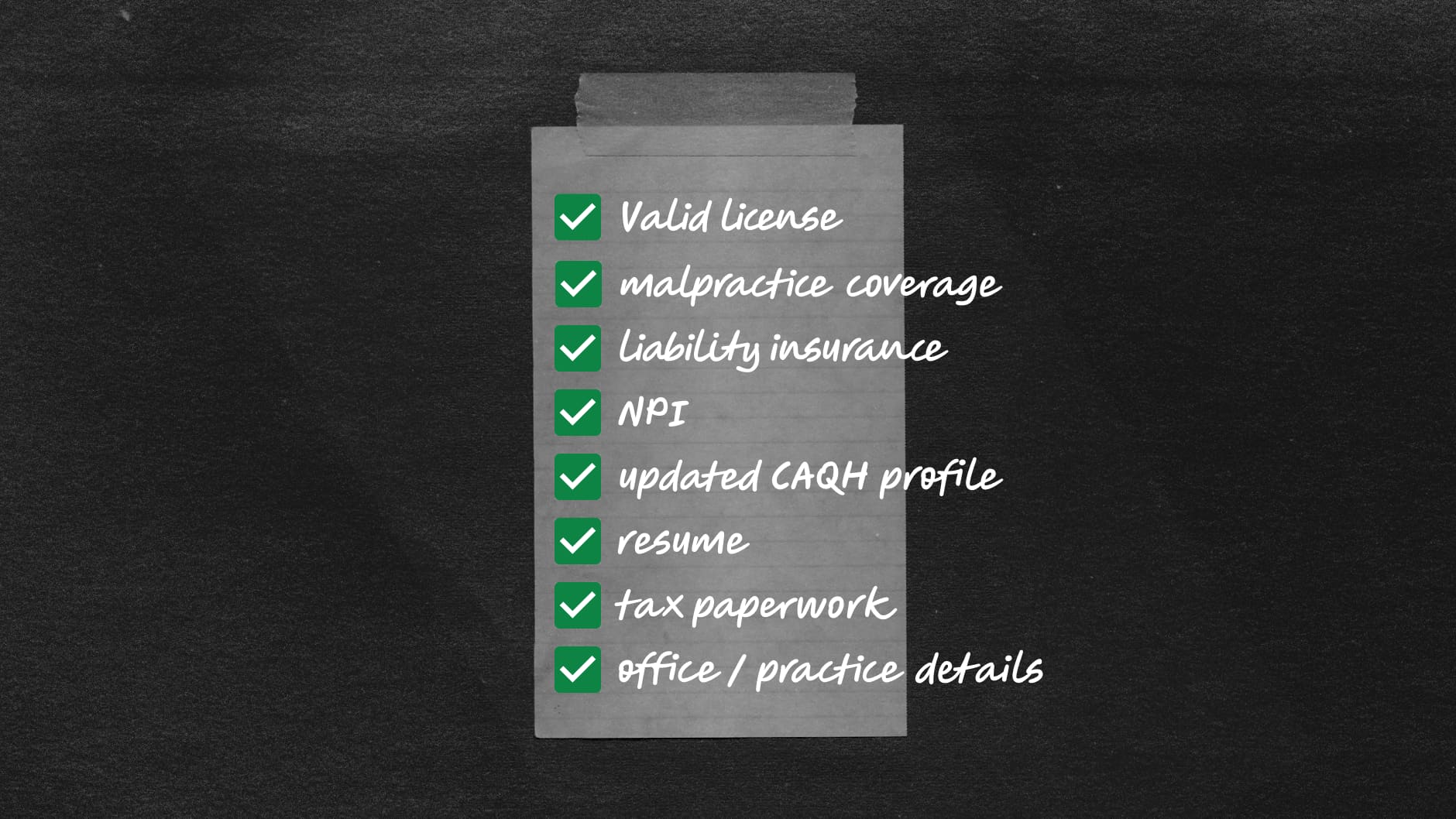
Insurers don’t necessarily tell you this explicitly, but the requirements are largely standardized across companies. They want:
- A valid, unrestricted license
- Proof of malpractice coverage
- Proof of liability insurance covering rental property (if applicable)
- Your NPI (Type I for individual providers, Type II for group practices)
- An updated CAQH profile, attested every 120 days
- Your CV or resume with every work gap explained
- Tax paperwork (EIN, W-9)
- Office/practice details (or proof of HIPAA-compliant telehealth platform)
So why do so many applications drag on? Because the smallest details can derail the process, like.
- Incomplete applications. A missing NPI or outdated malpractice certificate.
- Reference checks. If your references don’t respond quickly, the whole file sits untouched.
- Tax ID confusion. Applying under your SSN instead of an EIN, or listing a mismatch between your CAQH and license address.
- Panel “capacity.” Even when denied, providers sometimes find acceptance later if they highlight specialties insurers lack.
It’s the kind of red tape that leaves you staring at your inbox, wondering whether your entire career trajectory is hinging on a mis-typed digit.
It sounds straightforward, but the stumbling blocks are usually in the details, whether it is an expired malpractice certificate, a CAQH profile not properly attested (you can login to your CAQH Provider Data Portal here to do so), or a mismatch between your license and address. These tiny discrepancies are what gum up the works.
A Checklist to Keep Things Moving
If you can’t shrink the backlog, you can stop your own application from landing at the bottom of the pile. Here are a Prfew steps you can take to stack the odds in your favor.
Prep Your Documents in Advance
- Current license
- Proof of malpractice insurance meeting panel requirements
- Resume or CV with no unexplained gaps
- NPI Type I (and Type II if applicable)
- W-9 form with correct EIN
- Voided check for direct deposit
- Updated CAQH profile
Keep CAQH Updated
This is the single biggest stumbling block. You are required to update and attest every 120 days. Double-check your service locations, license numbers, and specialties match across all documents.
Follow Up Consistently
Do not submit and disappear. Call credentialing departments every 2–3 weeks. Log names, dates, and reference numbers. If state law guarantees a credentialing timeline, use that as leverage in your follow-up.
Apply Widely but Strategically
Don’t waste hours paneling with every insurer in existence. Instead, target those with high market share in your area. Apply to a few simultaneously, so a closed panel or long delay doesn’t stall your entire insurance strategy.
Know Your State Laws
California is in the midst of passing legislation that would require health care service plans and insurers to complete provider credentialing within 90 days. Illinois requires 60 days. Other states have variations. Knowing your rights changes your tone: you’re not begging, you’re holding insurers accountable.

What You Can Control (and What You Can’t)
It’s worth noting the cruel irony: insurers make it difficult for therapists to join their networks at the very moment when demand for mental health care has surged. More than 50 million U.S. adults experience mental illness each year, but only about 50% don’t receive treatment (SAMHSA, 2022). Meanwhile, clinicians willing to take insurance face barriers just to get in the door.
You can’t solve that contradiction alone. But by approaching the panel application process strategically, you can shorten your timeline, reduce your stress, and get to the part that actually matters: offering care. You can’t eliminate insurer backlogs. You can’t force them to declare panels “open.” You can’t fix the fact that credentialing departments are often underfunded and understaffed. However, you can control whether your CAQH profile is complete. You can control how often you follow up. You can control whether your documents line up exactly across applications. And you can control how widely you apply.
Most importantly, you can remind yourself: none of this is about your clinical value. It is not about your expertise, your capacity to help clients, or your worth as a provider. It’s about bureaucracy.
Always Aim to Be Strategic
Insurance panels may always feel more like gatekeeping than a gateway. But you can move from feeling at the mercy of silence to approaching the process with clarity. Treat your application like infrastructure-building: frustrating, yes, but essential to your practice’s long-term stability.
And remember: you’re not just credentialing for yourself. Every week insurers delay you is another week your future clients wait for care. You’re building systems that let you focus less on paperwork and more on therapy. In a system that thrives on opacity, persistence and preparation are your most radical tools.