In Brief
For therapists, clinical documentation is more than a bureaucratic necessity. It’s the scaffolding that supports continuity of care, protects client safety, and fulfills legal and insurance obligations. DAP notes, in particular, offer a structured yet flexible way to capture the arc of a therapy session: what happened, what it meant, and what’s next.
Yet, even the most dedicated clinicians will admit that note-writing often stretches past the end of the workday, bleeding into evenings and weekends. The challenge is twofold: being thorough enough to satisfy clinical and compliance standards, while being efficient enough to preserve your own work-life balance.
This is where both skill and technology come into play. If you’re new to DAP notes, start with our complete guide to writing DAP notes. In this guide, we’ll take a deep dive into advanced DAP note techniques, compare them to other formats, provide real-life examples across clinical contexts, and show how Blueprint AI can help you produce precise, audit-ready notes in a fraction of the time, all without sacrificing quality or your own professional voice.
Main Takeaways
- Small wording changes can transform a subjective impression into an objective, audit-ready statement.
- DAP notes are most effective when linked directly to treatment goals and measurable outcomes.
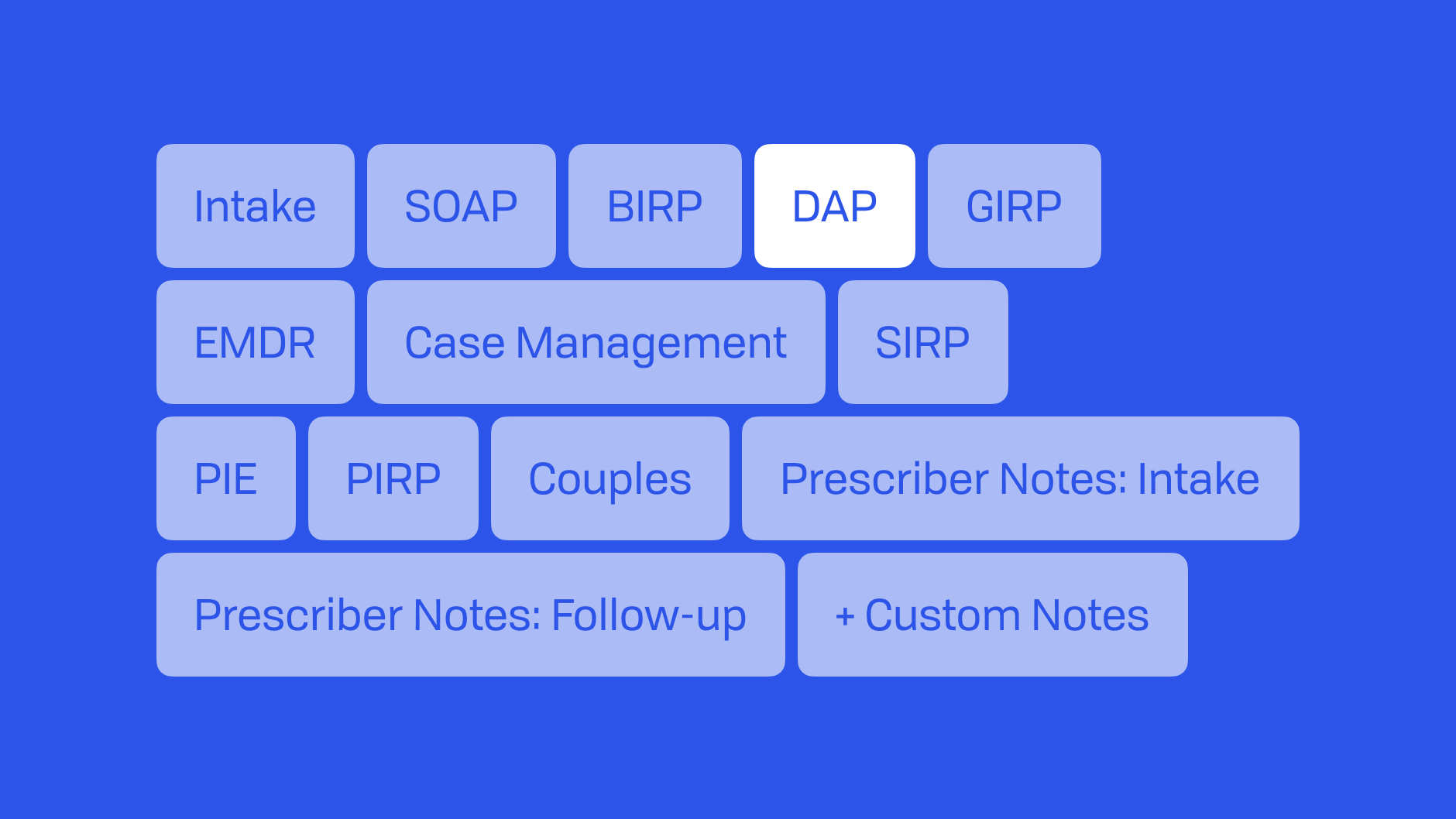
- Choosing between DAP and other formats (SOAP, BIRP, DARP) depends on your setting, diagnosis, and reporting needs.
- Real-world examples can guide your language, tone, and structure for different clinical contexts.
- Blueprint AI can cut your documentation time from hours to minutes while keeping your notes compliant and connected to treatment plans.
What Are DAP Notes?
DAP stands for Data, Assessment, and Plan: three concise sections that collectively summarize the most clinically relevant aspects of a session.
Unlike SOAP notes, which separate subjective and objective information, DAP notes consolidate observable facts into a single Data section. This makes them leaner than SOAP but still more comprehensive than informal narrative notes.
Why therapists choose DAP:
- Balance of brevity and completeness: enough structure to guide thinking without the time demands of SOAP.
- Audit readiness: each section maps to compliance expectations.
- Flexibility: adaptable for individual, group, or family therapy sessions.
With Blueprint, this structure becomes even more powerful: session transcriptions, progress measure integration, and treatment plan linkage mean you’re not starting with a blank page. It means you’re refining a clinically solid draft.
Core Components: Data, Assessment, Plan
D: Data
- Definition: Objective, factual observations from the session.
- Example: “Client presented with tearfulness, minimal eye contact, and soft speech.”
- Audit Tip: Include measurable or observable behaviors rather than interpretations. For more guidance on foundational communication skills, see Core Counseling Skills Every Therapist Should Strengthen.
- Pro Tip: Avoid interpretation here and reserve that for the Assessment section. Instead of “appeared anxious,” note observable signs: “tapped foot continuously, avoided direct gaze, and spoke in a rapid tone.”
- How Blueprint Helps: Blueprint captures a transcript of the session and can identify key behaviors, interventions, and client's direct quotes, pulling them directly into your Data section for you to review and approve.
A: Assessment
- Definition: Your professional interpretation of the data, linking it to diagnosis, functional impairment, treatment goals, or progress.
- Example: “Client’s presentation consistent with moderate depressive symptoms; improvement noted in energy level compared to prior session.”
- You can enhance this section by integrating measurement-based care.
- Pro Tip:
Standardized measure outcomes are recorded here. These are especially helpful in tracking client progress and can be used when working with insurers or multidisciplinary teams. Consider using measures to reference progress against SMART goals or identify specific therapeutic milestones. - How Blueprint Helps:
If you administer measures like the GAD-7, PHQ-9, or PCL-5 through Blueprint, the results appear in your account with date comparisons and are inserted directly into your note draft, saving you from manually digging through files.
P: Plan
- Definition: Next steps and interventions, including homework, referrals, or follow-up strategies.
- Example: “Introduce behavioral activation worksheet; review in next session.”
- For diagnosis-specific planning, see our Anxiety Treatment Plan Guide or ADHD Assessment and Treatment Guide.
- Pro Tip: Tie the plan directly to the assessment section and progress notes to help the note show clinical reasoning. This strengthens both your care and your defensibility in audits.
- How Blueprint Helps: Blueprint links your Plan section to treatment goals, past sessions, assessments, and client homework. You can pull forward previous interventions or automatically insert recommended evidence-based strategies based on session content.
DAP vs. Other Note Formats: How to Choose
DAP: Balanced documentation across observation, interpretation, and next steps (moderate detail)
- Pros: Efficient, easy to audit
- Cons: Less detailed than SOAP for complex cases
SOAP: Medical-model detail across Subjective, Objective, Assessment, and Plan (high detail)
- Pros: Comprehensive, widely recognized
- Cons: More time-consuming
BIRP: Focused on behavior, interventions, response, and plan (moderate detail)
- Pros: Tracks intervention outcomes clearly
- Cons: Less narrative flexibility
DARP: Data, Assessment, Response, and Plan (moderate detail)
- Pros: Captures client response explicitly
- Cons: Slightly more complex than DAP
For deeper format comparisons, explore our full guides to SOAP notes, BIRP notes, and therapy note best practices.
Blueprint’s advantage: Regardless of your preferred format, Blueprint can auto-generate notes in that style from the same source session, making it easy to switch formats based on setting or requirement.
How To Write Clinically Precise DAP Notes
Write With Clinical Precision
- Vague: “Client seemed upset and withdrawn during most of the session.”
- Precise: “Client presented with tearfulness, crossed arms, and short, one-word responses.”
Use Observable, Audit-Ready Language
Swap vague language for measurable descriptors. Avoid “appeared angry” in favor of “spoke in a raised voice and interrupted multiple times.”
Integrate Standardized Measures Strategically
Tie note content to SMART goals and interventions. For example, if using a PHQ-9, note: “Score decreased from 16 to 12 since last session. Therapist observed alignment with decrease in score and client reported increased activity engagement per behavioral activation plan.”
Blueprint AI makes this easier by automatically linking measures to your notes—see our guide on measurement-based care.
Self-Audit for Risk and Readability
- Are your interventions supported by your assessment?
- Have you avoided personal opinions or speculative language?
- Does the note meet compliance and timeliness requirements?
- Does your note demonstrate that the services are medically necessary?
Customize Structure Based on Diagnosis or Setting
- ADHD: Emphasize behavioral observations and task engagement (ADHD guide here).
- Trauma: Document emotional states and triggers with sensitivity (Trauma-informed approaches for veterans).
- Motivational Interviewing: Highlight client readiness and ambivalence (Motivational Interviewing guide).
Blueprint’s role: AI-generated notes can be instantly “Magic Edited” to change tone, add detail, or format for specific populations without rewriting from scratch.
7 Real-Life DAP Note Examples
Example 1: Anxiety Management
- D: Session conducted in person. Client reported experiencing increased anxiety over the past week, particularly due to stress about work deadlines, leading to feelings of being overwhelmed and difficulty sleeping. Therapist provided psychoeducation on mindfulness techniques and facilitated a deep breathing exercise to help the client manage their anxiety symptoms. During the session, the client appeared attentive and engaged, practicing the techniques with focus and expressing interest in incorporating them into their daily routine.
- A: Client is experiencing heightened anxiety, seemingly in response to external work-related stressors, resulting in sleep difficulties and feelings of being overwhelmed. Their motivation to adopt coping strategies discussed in previous sessions indicates a proactive approach to managing these symptoms. No suicidal or homicidal ideation was suspected or disclosed. The client did not make progress towards goal to improve sleep.
- P: Continue to practice grounding techniques regularly to manage anxiety symptoms. Schedule a follow-up session to review client’s progress and address ongoing challenges related to work stress.
Example 2: Depression Symptoms
- D: Client presented with a flat affect and expressed feeling, "I just feel numb." They reported a decrease in interest in previously enjoyable activities and an inability to complete tasks at work due to low motivation. The therapist facilitated behavioral activation by encouraging the client to increase engagement in meaningful activities, and used structured problem-solving interventions to support the client in enhancing task completion. Client appeared to be reflective during the session and acknowledged the impact of their symptoms on daily life.
- A: Client exhibits symptoms consistent with moderate depression, characterized by anhedonia, low motivation, and feelings of numbness, resulting in impairments at work and reduced engagement in pleasurable activities. These symptoms are indicative of the need for targeted interventions. No suicidal or homicidal ideation was suspected or disclosed. The client made no progress towards the goal as they continue to report difficulties with task completion at work.
- P: Introduce a weekly activity schedule to encourage client to partake in pleasurable activities and monitor mood changes. Follow up in the next session to evaluate the effectiveness of these strategies and adjust as needed.
Example 3: Grief and Loss
- D: Session conducted via telehealth. Client expressed profound sadness following the recent loss of a family member, noting difficulties with concentration and increased irritability as part of their grief experience. The therapist engaged the client in therapeutic exercises to facilitate the processing of this traumatic loss, creating a supportive environment for emotional exploration. Client participated openly, demonstrating a readiness to engage with the grieving process.
- A: Client is in the acute phase of grief, presenting with symptoms such as deep sadness, irritability, and trouble concentrating, impacting daily functioning. No suicidal or homicidal ideation was suspected or disclosed. These symptoms highlight the necessity for ongoing grief support and therapeutic intervention. The client reported some progress towards the goal of sorting through their loved one’s belongings for 10 minutes over the weekend.
- P: Explore grief processing techniques, such as journaling and support group options, to further assist client in managing their grief. A follow-up session is scheduled in two weeks to evaluate progress and refine therapeutic strategies.
Example 4: Self-Esteem Issues
- D: Session conducted in person. Client expressed feelings of inadequacy, citing frequent instances of negative self-talk, such as “I never do anything right.” They shared specific situations at work where they felt inadequate, emphasizing how these thoughts negatively impact their work performance and emotional well-being. Therapist utilized gentle cognitive challenging techniques to address client’s negative self-talk, identifying patterns of cognitive distortions and introducing the concept of cognitive reframing. The therapist also observed that the client appeared visibly disheartened when discussing their perceived failures, yet showed openness to exploring reframing techniques.
- A: The client’s low self-esteem appears to significantly affect their performance and overall well-being, contributing to feelings of inadequacy both professionally and personally. Symptoms of low self-worth, self-doubt, and persistent cognitive distortions were evident throughout the session. No suicidal or homicidal ideation was suspected or disclosed. Client's consistent cognitive distortions and negative self-perception indicate a need for focused cognitive restructuring interventions. The client did not make progress towards goal to increase meditation practice.
- P: Therapist will introduce cognitive restructuring exercises aimed at challenging the client’s persistent negative thoughts and cognitive distortions. Client and therapist agreed to schedule weekly check-ins to monitor client's progress and address any immediate challenges or changes in their thought patterns.
Example 5: ADHD Management
- D: Client expressed difficulties with focus and organization, primarily in the school environment, and reported feelings of being overwhelmed by tasks. The therapist facilitated a Brief Solutions-Focused Therapy intervention to help client recognize positive aspects and progress in school activities. Additionally, the therapist engaged client in a structured problem-solving intervention aimed at reducing obstacles to concentration in the school setting. Client participated actively and appeared motivated to improve organizational skills.
- A: Client's reported symptoms are indicative of ADHD, with challenges in focus, organization, and feelings of being overwhelmed. The client demonstrates eagerness to develop skills for improved focus and organization at school, highlighting a constructive attitude towards addressing these challenges. No suicidal or homicidal ideation was suspected or disclosed. The client reported minimal progress towards the treatment goal of completing homework before 9:00 pm.
- P: Collaborate with client on creating a personalized organizational system incorporating tools like checklists and timers. Review client’s progress and effectiveness of the strategies in the next session.
Example 6: Substance Use
- D: Session conducted in person. Client arrived late and disclosed daily alcohol use over the past week. Client reported drinking 3-4 beers per night along with a ‘night cap’ of 2 martinis. Client reported being unable to fall asleep without drinking and appeared tired with black circles under their eyes, rubbing their eyes and yawning frequently, and slowed reaction time when responding to questions. Client stated that increased work stress and social pressure contributed to alcohol use as well. Therapist conducted a brief motivational interviewing segment to explore the client's ambivalence about change and assessed immediate physical risk. Client expressed a desire to decrease alcohol use and find other ways to cope with stress.
- A: Presentation is consistent with alcohol misuse, with physical signs suggesting possible withdrawal risk. Contributing factors include occupational stress and environmental triggers. No suicidal or homicidal ideation was suspected or disclosed. Client’s relapse indicates regression from treatment goals, and a higher level of care is warranted.
- P: Refer client to inpatient detoxification for medical supervision. Establish daily phone check-ins for the next week to monitor withdrawal symptoms and emotional stability. Plan to initiate relapse prevention planning once medically stable.
Example 7: Trauma-Informed
- D: Session conducted via telehealth. Client displayed hypervigilance, including scanning the room repeatedly and reacting sharply to sudden background noises. When discussing past traumatic events, client avoided eye contact, became visibly tense, and had difficulty maintaining steady speech. Therapist implemented grounding techniques in session and discussed the option of introducing a trauma narrative in the future.
- A: Client’s symptoms are consistent with post-traumatic stress disorder (PTSD), including hyperarousal, avoidance, and re-experiencing triggers. Distress level was self-reported at 8/10. No suicidal or homicidal ideation was suspected or disclosed. These symptoms reflect ongoing difficulty managing trauma-related triggers and reinforce the need for structured trauma-focused intervention. Client reported no progress toward treatment goal to decrease avoidance behaviors.
- P: Continue grounding exercises between sessions, with daily practice logs. Plan to introduce a trauma narrative within 2–3 sessions, ensuring client readiness is reassessed each time. Encourage the client to identify and document potential triggers to review in the next session.
Streamline DAP Notes With Blueprint AI
Blueprint AI is more than a documentation tool. It is a clinically informed partner that bridges the gap between structured note-taking and automation. Designed specifically for mental health professionals, it helps you create compliant, goal-connected DAP notes in minutes while keeping full control over clinical decisions.
Document in Real Time Without Missing a Word
From the moment you log in, you can start recording session audio or use Blueprint’s telehealth video link for remote sessions. The AI assistant transcribes in real time and surfaces key clinical details, such as panic attack symptoms, safety plan updates, and grounding techniques interventions, directly into the Data, Assessment, and Plan fields. This ensures you capture nuance as it happens, not hours later.
Once your DAP note is complete, you can instantly generate treatment recommendations tailored to the session content. If no previous treatment plan had been established, the Plan section includes recommended objectives and interventions based on what was discussed, which you can review and refine to ensure it aligns with your clinical judgment and the client’s ongoing mental health goals and needs.
Generate Notes in Minutes, Not Hours
By the end of the session, your note is already drafted. You can choose to copy the AI’s output as-is or refine it. The Magic Edit feature, which lets you type instructions such as “remove all direct quotes” or “list all symptoms with frequency and severity” will make changes for the current and all existing future notes to learn your personalized style of writing notes. The AI will make the changes instantly. If you’d like to apply edits to a single note, simply type the changes you would like into the note and it will be autosaved. Either way, you have consistent control over tone, detail, and compliance.
Keep the Progress Intact
Blueprint automatically links your notes to prior treatment plans, worksheets, and assessments such as OASIS or CBT Thought Records so you can see progress in context. The Assist panel recommends evidence-based interventions, such as DBT TIPP skills, or related worksheets or assessments, based on the session content.
Support Risk and Readability Self-Audits
Before finalizing, Blueprint makes it easy to scan for vague or non-compliant language. You can use edit to correct unclear terms, check for measurable descriptors, and confirm your interventions align with your assessments and goals, helping you maintain both clinical accuracy and audit readiness.
Built-in Privacy and Control From Start to Save
Every note is created in a secure, HIPAA-compliant, SOC 2-certified environment. Once transcription is complete, recordings are permanently deleted, and you have full control over how long client data is stored. You remain the decision-maker for all clinical care while Blueprint handles the administrative load, giving you more time for client connection.
Do the Work You Love, We’ll Handle the Notes
DAP notes are powerful tools for organizing clinical thinking and ensuring quality care but they shouldn’t consume your evenings. By combining best practices with automation, Blueprint AI helps you create precise, compliant notes in a fraction of the time.
Start your free Blueprint trial today and see how easy documentation can be.
FAQs About DAP Notes
How long should a DAP note be?
Long enough to capture clinically relevant information while remaining concise, usually 1–2 short paragraphs per section.
What’s the difference between DAP and SOAP notes?
SOAP adds a “Subjective” section, which captures client-reported experiences separate from observable data. See our SOAP notes guide.
Is it okay to use client quotes in the Data section?
Yes, direct quotes can strengthen the factual basis of your notes, especially if relevant to treatment or risk assessment.