In Brief
In every therapist’s mission to provide the best, most impactful care possible for their clients, being thorough and accurate in your documentation is key. There are over a dozen note types to choose from for progress notes, but this guide will focus on the SOAP notes format, and how it can provide a structured framework to capture essential information about your clients' experiences, progress, and treatment plan in a comprehensive, consistent, and compliant way.
What are SOAP Notes?
In short, SOAP notes are a structure for documentation of therapy sessions. They consist of four sections: Subjective, Objective, Assessment, and Plan. SOAP notes were developed in the 1960s by Dr. Lawrence Weed as part of the problem-oriented medical record system. The structure of the format enables seamless communication among healthcare providers and ensures comprehensive patient records. Their clarity and organization promote consistency in clinical documentation, ultimately improving patient care and facilitating collaboration among multidisciplinary teams.

Benefits of SOAP Notes
Compared to other formats, SOAP notes are detailed and provide a well-rounded view of the client's condition. This format is particularly useful for:
- Comprehensive Documentation: SOAP notes capture both subjective experiences and objective observations, allowing for more in-depth records.
- Consistency: The structured format ensures all essential aspects of the client's condition and treatment are consistently documented.
- Insurance Compliance: SOAP notes meet common documentation requirements set by insurance providers, aiding in reimbursement and claim processes.
- Clarity for Multidisciplinary Teams: When working as an integrated team, the detailed sections make it easier for other healthcare providers to understand and act upon the client's progress and treatment plan.
Overall, SOAP notes are a great way for therapists to be both thorough and clear in their documentation, making it easier for them and their client’s larger treatment team to track and review client progress over time.
How to Write SOAP Notes
The structured format of SOAP notes is designed to capture essential information in a clear and concise manner. When writing SOAP notes, it's crucial to maintain clarity and precision in each section, ensuring that the information is easily understandable and actionable for both yourself and other healthcare professionals who may review the notes.
Step 1: Subjective
This is where you’ll document the client's reported experiences, feelings, and symptoms. Include direct quotes to capture the client's perceptions and concerns accurately. This section helps to provide a firsthand account of the client's experience and can be valuable for tracking progress over time. SOAP notes examples counseling can illustrate common entries and help guide your documentation.
Step 2: Objective
Next, record observable and measurable data from the session. This includes factual information like the client's physical appearance, behavioral observations, and any standardized assessment results. Using standardized tools can help ensure consistency and accuracy in your documentation.
Step 3: Assessment
Building on your observations, analyze and synthesize the subjective and objective data to provide a professional evaluation of the client's condition. This is where you can draw connections between the client's reported experiences and your objective observations, offering insights into their progress and any potential challenges. The assessment section is where you should include a sentence or two regarding the client’s progress towards their identified treatment goal.
Step 4: Plan
Finally, this section outlines the next steps in treatment based on your assessment. This includes setting therapeutic goals, determining appropriate interventions, and making any necessary adjustments to the existing treatment plan. Be specific and actionable in your planning, ensuring that the steps are clear and measurable.

When to Use SOAP Notes
When considering which note format is best for a client or situation, SOAP notes are ideal for sessions requiring comprehensive documentation. This format is particularly effective in:
- Detailed Progress Notes: SOAP notes offer a thorough structure for documenting initial and comprehensive assessments.
- Complex Cases: When a client's symptoms or treatment needs are complex, SOAP's detailed breakdown supports deeper analysis.
- Multidisciplinary Settings: SOAP notes facilitate communication across various care teams by organizing detailed, structured information.
Using SOAP notes in scenarios like these allows for a robust record of client conditions, progress, and next steps. But like any other format, consider what style of documentation aligns best with the goals of the session.
Examples of SOAP Notes
Depression Symptoms
- Subjective: Client reports feeling "overwhelmed" and "hopeless" since last week. States that they are struggling to get out of bed and have lost interest in activities they used to enjoy, like reading and socializing. They express frustration with their lack of motivation and mention negative self-talk, saying, "I'm just not good enough." The client also describes difficulty sleeping, averaging 4-5 hours per night.
- Objective: Client appeared fatigued but engaged during the session. Affect was flat, and mood was reported as "low." They maintained eye contact and were cooperative. No signs of psychomotor agitation or retardation noted. Homework from the previous session (thought records) was partially completed; client shared a few examples of negative automatic thoughts and their cognitive distortions. Therapist engaged client in discussion on negative self-talk, including provided psychoeducation cognitive distortions. Therapist supported client in identifying and reframing cognitive distortions as they were happening in session.
- Assessment: Client is demonstrating symptoms consistent with Major Depressive Disorder. The negative thought patterns identified suggest cognitive distortions such as all-or-nothing thinking and catastrophizing. The client's engagement in therapy is a positive sign, though ongoing feelings of hopelessness and low motivation indicate a need for continued support and skills practice. The client reports no progress towards goal to improve sleep.
- Plan: Continue with CBT techniques to challenge negative thoughts and cognitive distortions. Assign homework to complete a thought record for at least three different instances of negative thinking this week. Introduce behavioral activation strategies to encourage engagement in pleasurable activities, starting with one activity they used to enjoy. Schedule a follow-up session for one week to assess progress and adjust the treatment plan as needed.

Acute Panic Session
- Subjective: Client reports experiencing a panic attack last night while watching television, describing symptoms such as rapid heart rate, shortness of breath, dizziness, and a feeling of impending doom. They expressed fear of having another attack and stated, "I feel like I'm losing control." The client mentioned avoiding places where previous attacks occurred, which is impacting their daily activities, including work and social outings.
- Objective: Client appeared visibly anxious during the session, with fidgeting and rapid speech. Affect was anxious, and they exhibited signs of distress when discussing the panic attack. Breathing was slightly elevated at the beginning of the session but calmed as the session progressed. No physical signs of hyperventilation were observed.
- Assessment: Client is experiencing acute panic episodes, the avoidance behavior is beginning to limit their functioning in daily life, suggesting an escalation in anxiety. The client's insight into their symptoms is positive, and they are motivated to develop coping strategies. The client is not making progress towards goal to decrease panic attacks.
- Plan: Introduce breathing techniques to manage acute anxiety symptoms, focusing on diaphragmatic breathing. Discuss cognitive restructuring to challenge irrational thoughts associated with panic attacks. Plan to implement gradual exposure to feared situations, starting with less anxiety-provoking environments. Schedule a follow-up session in one week to monitor progress and adjust interventions as necessary.
Common Pitfalls in SOAP Note Writing
While SOAP notes offer a structured approach to documentation, there are a few common pitfalls that can reduce their effectiveness. Here are some key things to avoid:
- Too Much Subjectivity in the Objective Section: The Objective section should focus on measurable, observable data. Be cautious not to include interpretations or subjective impressions in this section, as it can blur the line between factual information and opinion.
- Inconsistent Assessments: Your Assessment should be directly linked to the Subjective and Objective data presented in the note. Aim to avoid making assessments that are not supported by the information gathered during the session, as this can lead to confusion and inconsistency in treatment planning.
- Vague Plans: The Plan section should be specific, with clear, actionable steps that contribute to the client's overall treatment goals. Avoid generic or vague statements that do not provide a concrete direction for future sessions or interventions.
By being mindful of these common pitfalls, you can enhance the clarity, consistency, and effectiveness of your SOAP notes, ensuring that they serve as a valuable tool in supporting client progress and informing treatment decisions.

SOAP Notes Compared to Other Formats
While SOAP notes are widely used in various therapeutic settings, there are lots of other options at your disposal. Here are a few ways that SOAP compares to some other common formats you might be considering.
- DAP (Data, Assessment, Plan): DAP notes are a more concise version of SOAP notes, focusing on three main sections (essentially combining Objective and Subjective observations) This format is particularly useful for quick progress tracking and can be a good fit for therapists who prefer a streamlined approach to documentation.
- BIRP (Behavior, Intervention, Response, Plan): BIRP notes place a stronger emphasis on documenting specific behaviors, interventions, and client responses. This format is especially helpful for therapists who focus on behavioral health interventions and need to track the effectiveness of specific strategies.
Your choice between any documentation format depends on your practice's specific needs, the type of therapy you provide, and your personal preferences as a therapist, so it’s always worth comparing to find what’s best for your needs.
Frequently Asked Questions (FAQ)
What kinds of therapy are SOAP notes best suited for?
SOAP notes are versatile and can be used effectively in various therapeutic settings. They are especially well-suited for individual and family therapy sessions, where detailed documentation is needed to track progress and inform treatment planning – particularly in cases with complex or multiple presenting concerns.
How much detail should be included in SOAP notes?
Aim to include relevant details that support your assessment and treatment plan without overwhelming the record with unnecessary information. Each section should cover the key points that directly contribute to understanding the client's current status, progress, and future direction. Try your best to strike a balance between thoroughness and conciseness to ensure that your notes are informative yet manageable.
Can SOAP notes be used for group therapy?
Absolutely, SOAP notes can be adapted for use in group therapy settings. When documenting group sessions, be sure to capture both individual observations and group dynamics. Then, tailor each section of the SOAP note to reflect insights about each group member's participation, progress, and challenges, while also noting overall group themes and interactions.
How do SOAP notes meet insurance requirements?
When properly written, SOAP notes meet many insurance documentation standards. The comprehensive nature of SOAP notes allows therapists to demonstrate medical necessity, track treatment progress, and justify the need for ongoing services. By including relevant details in each section, like noting therapist contribution to session or any interventions done in session, and tying the assessment and plan directly to the client's presenting concerns and treatment goals – SOAP-formatted documentation can support seamless insurance reimbursement and ensure compliance.
Final Thoughts on SOAP Notes
Mastering the SOAP note framework offers a structured, comprehensive, yet versatile approach to documenting therapy sessions, making them an ideal choice for clinicians who require detailed, organized records to support their work. As compared to other documentation styles, SOAP notes can enhance the quality of your notes, ensure compliance with industry standards, and ultimately promote better continuity of care for your clients.
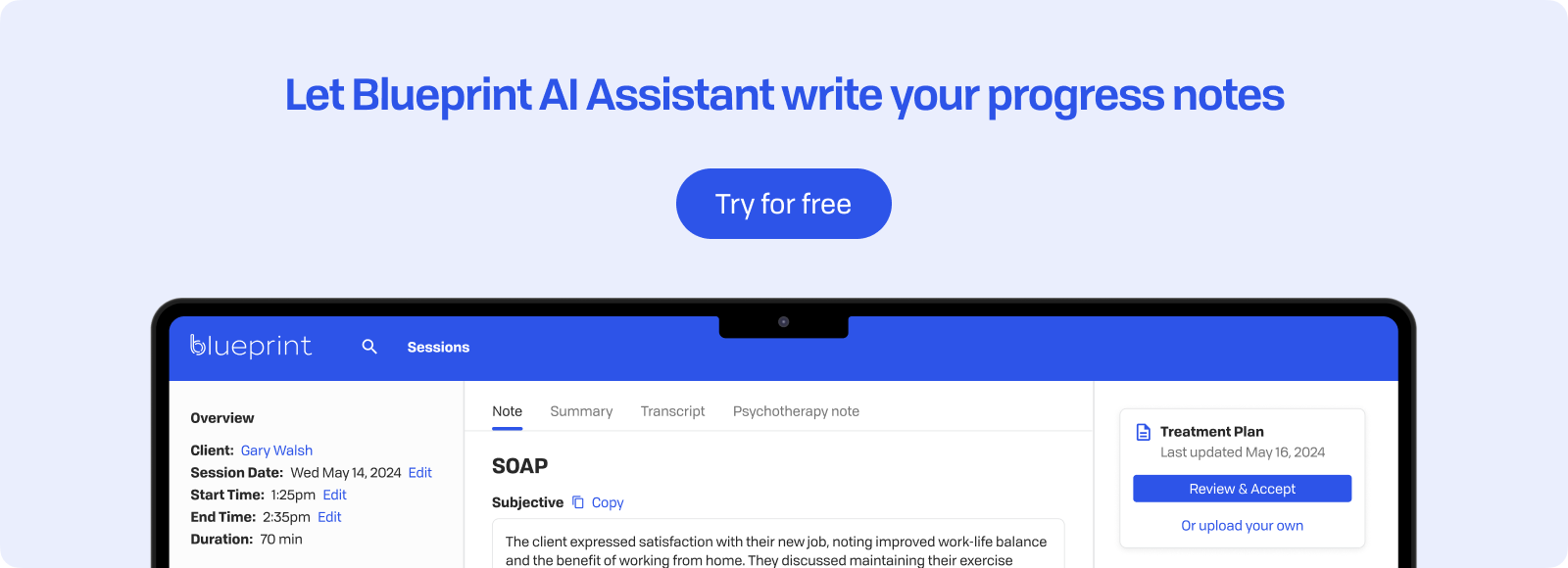
How Blueprint can help streamline your workflow
Blueprint is a HIPAA-compliant AI Assistant built with therapists, for the way therapists work. Trusted by over 50,000 clinicians, Blueprint automates progress notes, drafts smart treatment plans, and surfaces actionable insights before, during, and after every client session. That means saving about 5-10 hours each week — so you have more time to focus on what matters most to you.
Try your first five sessions of Blueprint for free. No credit card required, with a 60-day money-back guarantee.
























