In Brief
Writing progress notes is not only essential for providing the highest quality care for your clients, but ensuring that all insurance companies and other institutions have what they need. When thoroughness is top of mind, SOAP notes provide a structured framework to capture the essential elements of each therapeutic encounter, ensuring clarity, consistency, and continuity of care with other healthcare professionals.
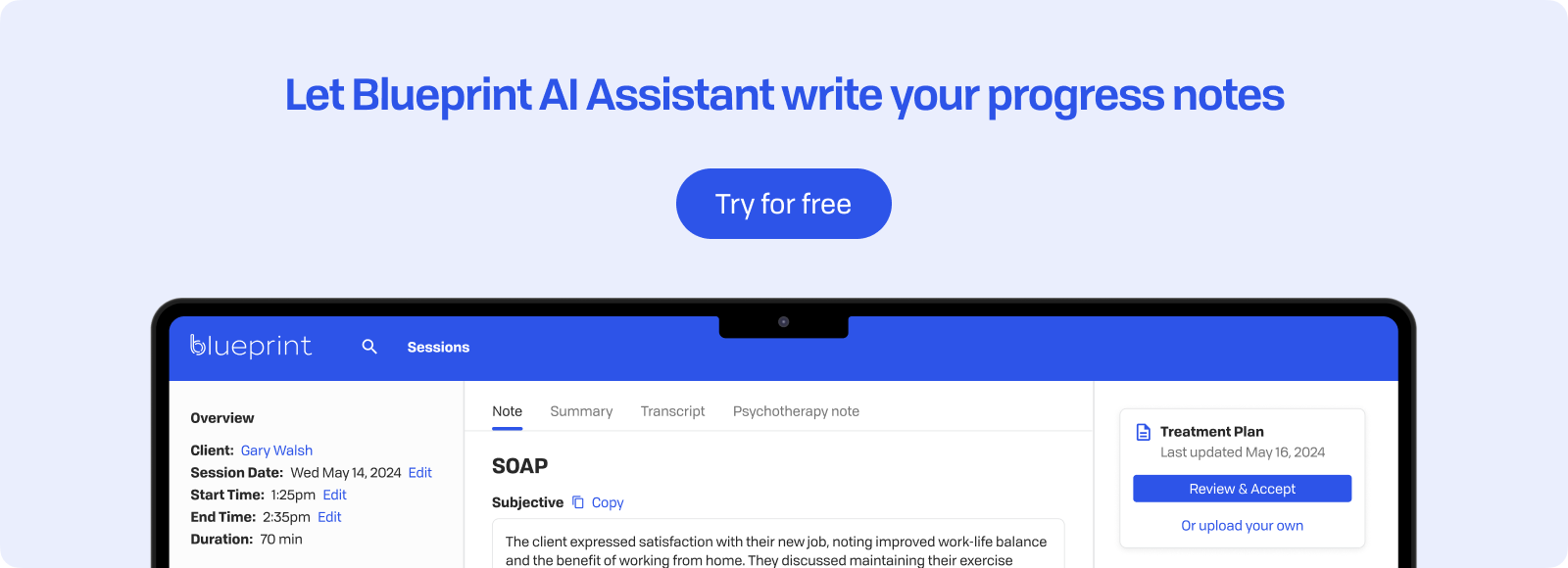
Let’s jump into SOAP notes, exploring the key components, basic format, and practical examples tailored specifically for mental health therapists and other clinicians. If you’d also like a more comprehensive guide to SOAP notes, and a way to auto-generate SOAP notes (or 15+ other formats), we’ve got that too.
What are SOAP Notes?
The basic structure of SOAP notes are: Subjective, Objective, Assessment, and Plan. This standardized format ensures that mental health professionals capture clear, consistent, and comprehensive information about each client encounter – and allow for better collaboration with other interdisciplinary clinicians. Let’s explore each section:
- Subjective: The Subjective section captures your client's reported symptoms, feelings, and experiences in their own words. This section should include relevant quotes, paraphrases, and summarized statements that provide insight into the client's perspective on their progress, challenges, and goals. By documenting the client's subjective experience, you can gain a deeper understanding of their unique struggles and successes, which can inform your treatment planning and interventions.
- Objective: Here, you’ll document observable, measurable, and factual data from the session. This may include your observations of the client's appearance, behavior, and affect, any provider interventions and how they target client’s reported symptoms, as well as the results of any assessments, tests, or scales administered during the session. By focusing on objective data, you can provide a more accurate and unbiased account of the client's presentation, which can be especially valuable when collaborating with other healthcare professionals or justifying treatment decisions.
- Assessment: This section is where you’ll synthesize your clinical impressions, insights, and interpretations based on the information gathered in the Subjective and Objective sections. This may include diagnostic considerations, updates to the treatment plan, and an integration of the subjective and objective data to inform clinical reasoning. This is the section where you should include a sentence or two on the client’s progress towards their identified treatment goal. By clearly articulating your assessment, you can demonstrate your expertise and provide a rationale for treatment recommendations.
- Plan: Finally, you’ll outline the next steps, interventions, and goals for upcoming sessions. This may include specific therapeutic techniques, referrals to other healthcare providers, coordination of care, and follow-up tasks. Additionally, you can consider including recommendations for client homework or self-care activities to be completed between sessions. By documenting a clear and actionable plan, you can ensure continuity of care and help clients stay on track with their goals.

Tips for writing effective SOAP notes
- Be Clear and Concise: Use straightforward language and avoid jargon. Focus on capturing essential information without unnecessary detail. This helps ensure that your notes are easily understood by anyone who might read them.
- Stick to the Facts: Avoid any personal opinions or assumptions when noting objective observations and client’s subjective experiences. Let the data speak for itself: try to use specific examples and quotes from the client to support your entries.
- Use a Consistent Format: Maintain a uniform structure for your SOAP notes: this consistency makes it easier to track client progress over time and helps other healthcare professionals quickly understand context.
- Focus on Clinical Relevance: Each section (Subjective, Objective, Assessment, Plan) serves a clear clinical purpose when it comes to clinical relevance. For instance, your assessment should directly link to and build from the data collected in the subjective and objective sections, guiding the plan for treatment.
- Review and Revise: Before finalizing your notes, take a moment to proofread for clarity and accuracy. This helps prevent misunderstandings and ensures your notes meet legal and compliance standards, which is especially important in insurance and legal contexts.
SOAP Note Examples
Whether you're a seasoned practitioner or just starting out in your career, how the SOAP format looks across a number of client concerns, diagnosable conditions, and therapeutic approaches can help you refine your documentation skills and ensure compliance with industry standards.
Example 1: Anxiety Management
S: Session conducted via telehealth. Client reported increased anxiety over the past week, particularly about work deadlines, feeling overwhelmed and having difficulty sleeping. Client stated, "I just can't shut my brain off at night."
O: Therapist utilized cognitive restructuring to challenge the client's catastrophic thinking patterns regarding work deadlines. Therapist also introduced mindfulness exercises to help the client manage anxiety symptoms, such as racing thoughts and difficulty sleeping.
A: Client reports heightened anxiety symptoms, including racing thoughts, restlessness, feelings of being overwhelmed, and difficulty sleeping, likely due to external stressors related to work. These symptoms have resulted in impaired functioning, as the client has reported difficulties concentrating and decreased productivity at work. No suicidal or homicidal ideation was suspected or disclosed. The client reported no progress towards goal to improve sleep.
P: Client will practice mindfulness exercises before bedtime to help with sleep and will use cognitive restructuring techniques to challenge catastrophic thoughts. A follow-up session will be scheduled to review progress on managing work-related stress.

Example 2: Depression Symptoms
S: Session conducted in-office. Client presented with a flat affect and stated, "I just feel numb." They reported a decrease in interest in activities they once enjoyed, such as painting and socializing with friends. Client also reported feelings of hopelessness and difficulty concentrating.
O: Therapist utilized cognitive behavioral therapy (CBT) techniques, including cognitive restructuring, to address the client's negative thought patterns. Therapist discussed behavioral activation strategies to increase client’s engagement in previously enjoyable activities. Additionally, guided imagery was introduced to help the client visualize positive outcomes and alleviate feelings of hopelessness.
A: Client reports depressive symptoms, including flat affect, anhedonia, feelings of hopelessness, difficulty concentrating, and decreased interest in previously enjoyable activities, more days than not, resulting in social withdrawal and impaired daily functioning. The client's symptoms are consistent with moderate depression. No suicidal or homicidal ideation was suspected or disclosed. The client did not make progress towards their treatment goal of socializing with a friend once per week.
P: Client will implement a weekly activity schedule focusing on engaging in one pleasurable activity each day, such as painting or walking with friends. Client will also practice guided imagery exercises to combat feelings of hopelessness. Progress will be monitored in the next session to evaluate mood changes and engagement levels.
Example 3: Relationship Issues
S: Session conducted via telehealth. Client discussed ongoing conflicts with their partner, highlighting feelings of frustration and resentment. Client shared specific examples of miscommunication, stating, "We always end up arguing about chores that should just be simple."
O: Therapist utilized Gottman Method interventions, focusing on building the client's awareness of their emotional responses during conflicts. Therapist introduced the concept of gentle start-up to facilitate more constructive dialogue with their partner and practiced this through structured exercises in session. A brief role-playing exercise was conducted to reinforce positive communication patterns and repair techniques.
A: Client reports interpersonal stressors, characterized by frequent arguments, miscommunications, and feelings of frustration and resentment within their relationship. These difficulties in communication are significantly impacting relationship satisfaction and contributing to emotional distress. The client has reported increased anxiety and irritability related to these conflicts. No suicidal or homicidal ideation was suspected or disclosed. Client reported no progress towards goals to decrease arguing with spouse.
P: Client will implement the gentle start-up technique during discussions with their partner and will practice repairing interactions after conflicts. Therapist will facilitate additional role-playing in upcoming sessions to strengthen the client’s ability to manage and de-escalate conflicts. Progress will be assessed in the next session to evaluate improvements in relationship dynamics and emotional well-being.

Example 4: Grief Counseling
S: Session conducted in-office. Client shared their experience of losing a loved one, expressing profound feelings of sadness, loneliness, and difficulty accepting the loss. They reported trouble sleeping and a lack of motivation to engage in daily activities, stating, "Everything feels so empty without them."
O: Client appeared tearful and spoke with a flat affect when discussing their loss, indicating deep emotional distress. Therapist provided empathetic listening and supportive counseling, creating a safe environment for the client to express their grief openly. Therapist introduced initial elements of grief-focused therapy, including discussions around the process of meaning-making and memorialization, to help the client navigate their grief.
A: Client is experiencing normal grief reactions, including sadness, loneliness, sleep disturbances, and diminished motivation for daily activities. These symptoms are common responses to loss but contribute to a decrease in overall functioning. The client benefits from supportive counseling to process their emotions and find pathways to adapt to life without their loved one. No suicidal or homicidal ideation was suspected or disclosed. Client reported no progress towards goal to go on a walk once per week with a friend.
P: Continue to provide a safe and empathetic space for the client to express their grief. Encourage the client to engage in self-care activities and reach out to their support system for additional emotional sustenance. Incorporate further elements of grief-focused therapy, focusing on meaning-making and memorialization activities to aid in emotional processing and adjustment. Progress will be tracked in upcoming sessions as the client explores and integrates their grief.
Example 5: Trauma-Focused Therapy
S: Session conducted in-office. Client shared a vivid flashback of a traumatic event, expressing feelings of fear, helplessness, and guilt. They reported difficulty sleeping and concentrating due to intrusive thoughts. Client stated, "It's like I'm reliving it all over again every night."
O: Client appeared visibly distressed when recounting the traumatic memory, with trembling hands, a shaky voice, and tearfulness. Therapist implemented trauma-focused cognitive-behavioral therapy (TF-CBT) interventions, facilitating the client’s exploration of their thoughts and feelings associated with the trauma. Therapist introduced grounding techniques and guided relaxation exercises to help manage distress and reduce symptoms of hyperarousal.
A: Client exhibits symptoms consistent with post-traumatic stress disorder (PTSD), including vivid flashbacks, intrusive thoughts, hyperarousal, emotional distress, and sleep disturbances. These symptoms significantly impair the client’s daily functioning, including concentration and restful sleep. Client expressed feelings of fear, helplessness, and guilt further compound the emotional burden and distress. No suicidal or homicidal ideation was suspected or disclosed. The client reported a regression in progress towards goal of decreasing flashbacks.
P: Client will practice grounding techniques and relaxation exercises daily to manage distress and improve sleep quality. Therapist will integrate trauma-focused cognitive-behavioral therapy (TF-CBT) techniques in future sessions to further address and process traumatic memories. Progress will be closely monitored in the subsequent session to evaluate symptom reduction and emotional coping.

Integrating SOAP Notes into Your Practice
While any template you use can help provide a consistent structure that saves you time and mental energy, there are several strengths to the SOAP format. Applying SOAP notes in your documentation workflow can be an effective way to be tease out both objective and subjective observations for more comprehensive assessments and treatment planning. Beyond applying a consistent structure, be sure to regularly review and update your SOAP notes to accurately reflect your client’s progress and any changes in their treatment plan. Also ensure that your notes are stored securely in compliance with HIPAA regulations to protect your clients’ privacy.
In the spirit of conserving mental energy when it comes to doing your notes, consider exploring AI note-taking apps designed for therapists, which can help capture key points efficiently, allowing you to focus more on your clients.
All note formats have their particular strengths, and if being comprehensive and clear is important to you and valuable for your client session, using a SOAP format is worth considering.