In Brief
In running your practice, you’re already familiar with the process of writing therapy notes, and how they can be time-consuming and feel like a distraction from the meaningful work of helping your clients. That’s where DAP notes can shine: they offer a structured format designed to streamline your documentation process without sacrificing quality or compliance.
Let’s dive a bit more into DAP notes, exploring their components, benefits, various real-world examples, and practical tips to help you master this efficient note-taking technique. If you’d like a more in-depth guide to DAP notes, we’ve got you covered.
What are DAP notes?
Developing a keen understanding of this note structure will help you organize important information to be thorough, but efficient – all while satisfying requirements for compliance.
- Data: The data section of a DAP note is where you record measurable, objective information gathered during the session. This includes your client's presenting concerns, symptoms, and any relevant quotes or observations that provide insight into their current state. You may also include therapist intervention, and results from assessments or screenings administered during the session. This information will serve as the foundation for your assessment and treatment planning.
- Assessment: In the assessment section, you’ll provide your clinical analysis of your data you collected: interpreting the client’s progress, diagnosis, and potential risk factors. Because it developed off your objective data, your assessment strengthens the credibility of your conclusions and helps other healthcare professionals clearly understand your thought process. This section also includes a comment on the client’s progress toward their identified treatment goals.
- Plan: Building on your assessment, the plan section outlines the next steps in your client's treatment journey. This may include adjustments to their current treatment plan, specific homework assignments or interventions to try between sessions, setting clear and achievable goals, and scheduling future appointments. The plan should be tailored to your client's unique needs and goals, reflecting the insights gained from the data and assessment sections.

Tips for Writing Effective DAP notes
- Be concise: Focus on capturing essential information without getting bogged down in unnecessary details.
- Use clear language: Avoid jargon or overly technical terms, and aim for a professional tone that is easily understood by other healthcare providers.
- Stick to the facts: Refrain from including personal opinions or judgments in your notes, and instead rely on specific examples and observations.
- Ensure compliance: Make sure your DAP notes meet medical necessity documentation requirements set by insurance providers, including HIPAA regulations and professional standards of practice. This ensures that services are reimbursed without issues.
- Proofread: Always review your notes for accuracy and clarity before finalizing them, as mentioned above – they are often used for legal or insurance purposes.
DAP Note Examples
There’s of course no “one-size-fits-all” DAP note example, so we’ll explore several variations across different therapy types, client concerns, and diagnosable conditions, so you can better get a feel for how they function and sound.
Example 1: Anxiety Management
D: Session conducted in person. Client reported experiencing increased anxiety over the past week, particularly due to stress about work deadlines, leading to feelings of being overwhelmed and difficulty sleeping. Therapist provided psychoeducation on mindfulness techniques and facilitated a deep breathing exercise to help the client manage their anxiety symptoms. During the session, the client appeared attentive and engaged, practicing the techniques with focus and expressing interest in incorporating them into their daily routine.
A: Client is experiencing heightened anxiety, seemingly in response to external work-related stressors, resulting in sleep difficulties and feelings of being overwhelmed. Their motivation to adopt coping strategies discussed in previous sessions indicates a proactive approach to managing these symptoms. No suicidal or homicidal ideation was suspected or disclosed. The client did not make progress towards goal to improve sleep.
P: Continue to practice grounding techniques regularly to manage anxiety symptoms. Schedule a follow-up session to review client’s progress and address ongoing challenges related to work stress.

Example 2: Depression Symptoms
D: Client presented with a flat affect and expressed feeling, "I just feel numb." They reported a decrease in interest in previously enjoyable activities and an inability to complete tasks at work due to low motivation. The therapist facilitated behavioral activation by encouraging client to increase engagement in meaningful activities, and used structured problem-solving interventions to support client in enhancing task completion. Client appeared to be reflective during the session and acknowledged the impact of their symptoms on daily life.
A: Client exhibits symptoms consistent with moderate depression, characterized by anhedonia, low motivation, and feelings of numbness, resulting in impairments at work and reduced engagement in pleasurable activities. These symptoms are indicative of the need for targeted interventions. No suicidal or homicidal ideation was suspected or disclosed. The client made no progress towards goal as they continue to report difficulties with task completion at work.
P: Introduce a weekly activity schedule to encourage client to partake in pleasurable activities and monitor mood changes. Follow up in the next session to evaluate the effectiveness of these strategies and adjust as needed.
Example 3: Grief and Loss
D: Session conducted via telehealth. Client expressed profound sadness following the recent loss of a family member, noting difficulties with concentration and increased irritability as part of their grief experience. The therapist engaged the client in therapeutic exercises to facilitate the processing of this traumatic loss, creating a supportive environment for emotional exploration. Client participated openly, demonstrating a readiness to engage with the grieving process.
A: Client is in the acute phase of grief, presenting with symptoms such as deep sadness, irritability, and trouble concentrating, impacting daily functioning. No suicidal or homicidal ideation was suspected or disclosed. These symptoms highlight the necessity for ongoing grief support and therapeutic intervention. The client reported some progress towards goal of sorting through their loved one’s belongings for 10 minutes over the weekend.
P: Explore grief processing techniques, such as journaling and support group options, to further assist client in managing their grief. A follow-up session is scheduled in two weeks to evaluate progress and refine therapeutic strategies.

Example 4: Self-Esteem Issues
D: Session conducted in person. Client expressed feelings of inadequacy, citing frequent instances of negative self-talk, such as “I never do anything right.” They shared specific situations at work where they felt inadequate, emphasizing how these thoughts negatively impact their work performance and emotional well-being. Therapist utilized gentle cognitive challenging techniques to address client’s negative self-talk, identifying patterns of cognitive distortions and introducing the concept of cognitive reframing. The therapist also observed that the client appeared visibly disheartened when discussing their perceived failures, yet showed openness to exploring reframing techniques.
A: The client’s low self-esteem appears to significantly affect their performance and overall well-being, contributing to feelings of inadequacy both professionally and personally. Symptoms of low self-worth, self-doubt, and persistent cognitive distortions were evident throughout the session. No suicidal or homicidal ideation was suspected or disclosed. Client's consistent cognitive distortions and negative self-perception indicate a need for focused cognitive restructuring interventions. The client did not make progress towards goal to increase meditation practice.
P: Therapist will introduce cognitive restructuring exercises aimed at challenging the client’s persistent negative thoughts and cognitive distortions. Client and therapist agreed to schedule weekly check-ins to monitor client's progress and address any immediate challenges or changes in their thought patterns.
Example 5: ADHD Management
D: Client expressed difficulties with focus and organization, primarily in the school environment, and reported feelings of being overwhelmed by tasks. The therapist facilitated a Brief Solutions-Focused Therapy intervention to help client recognize positive aspects and progress in school activities. Additionally, the therapist engaged client in a structured problem-solving intervention aimed at reducing obstacles to concentration in the school setting. Client participated actively and appeared motivated to improve organizational skills.
A: Client's reported symptoms are indicative of ADHD, with challenges in focus, organization, and feelings of being overwhelmed. The client demonstrates eagerness to develop skills for improved focus and organization at school, highlighting a constructive attitude towards addressing these challenges. No suicidal or homicidal ideation was suspected or disclosed. The client reported minimal progress towards treatment goal of completing homework before 9:00 pm.
P: Collaborate with client on creating a personalized organizational system incorporating tools like checklists and timers. Review client’s progress and effectiveness of the strategies in the next session.

Integrating DAP notes into your practice
Incorporating DAP notes into your documentation workflow can help you streamline your practice and ensure that you're capturing all the essential information from each session. To make the process even more efficient, consider using templates that provide a consistent structure for your notes, saving you time and mental energy.
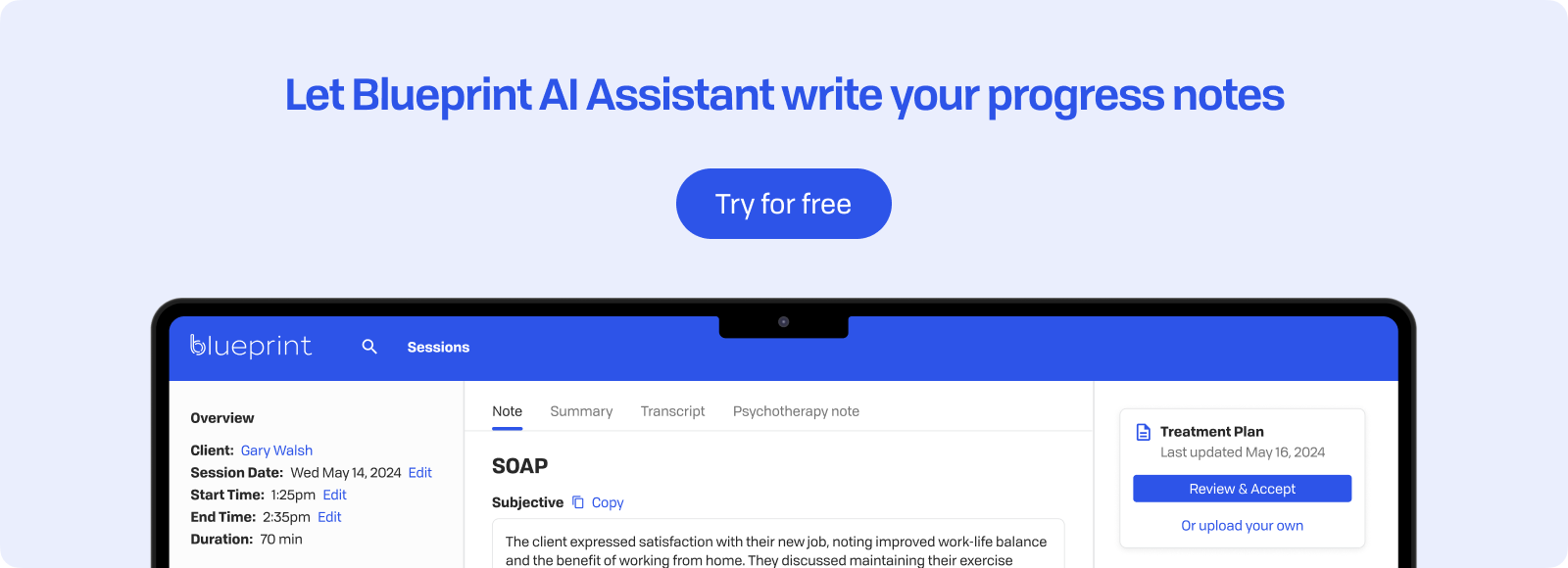
As technology advances, you may also want to explore AI note-taking apps designed specifically for therapists. These tools can help you quickly capture key points from your sessions, allowing you to focus more on your clients and less on documentation.
Remember to review and proofread from each session, ensuring that they accurately reflect your client's progress and any changes in their treatment plan. It's also crucial to store your notes securely, in compliance with HIPAA regulations, to protect your clients' privacy and maintain the integrity of your practice.
By mastering and including DAP notes into your workflow, you can create a more efficient and effective documentation process that supports your clinical work, allowing you to make a greater impact on your clients’ progress.